014 |
0 Commentaire
Recommandations 2014 pour la prise en charge de l’hyponatrémie
L’hyponatrémie est fréquente, mais sa prise en charge n’avait jamais l’objet d’un consensus d’expert. Plusieurs sociétés savantes (ESIM, ESE, ERA-EDTA (ERBP)) se sont regroupées pour élaborer des directives quant au diagnostique et au traitement de l’hyponatrémie vraie. Ces directives sont parues dans l’European Journal of Endocrinology en mars 2014.[1]
Cette prise en charge se focalise plus sur le patient que sur une valeur de laboratoire.[2]L’hyponatrémie est définie comme un sodium sérique (Na) inférieur à 135 mmol/l avec plusieurs degrés (légère, modérée, sévère)
| Légère | Na entre 130 et 135 mmol/l |
| Modérée | Na entre 125 et 129 mmol/l |
| Sévère | Na inférieur à 125 mmol/l |
L’hyponatrémie concerne jusqu’à 30% des patients hospitalisés.
Tout praticien hospitalier doit être en mesure d’en poser le diagnostic
précis, de la classer et de la traiter efficacement.
Par principe, il s’agit de traiter initialement l’hyponatrémie sévère indépendamment de la pathologie de base en évitant une correction trop rapide et en se concentrant davantage sur le patient que sur la valeur de laboratoire elle-même.Pour utiliser les 2 algorithmes suivants, outre les définitions
données plus hautes, il faut avoir examiné son patient et pouvoir
évaluer sa volémie (hypovolémique, euvolémique ou hypervloémique)
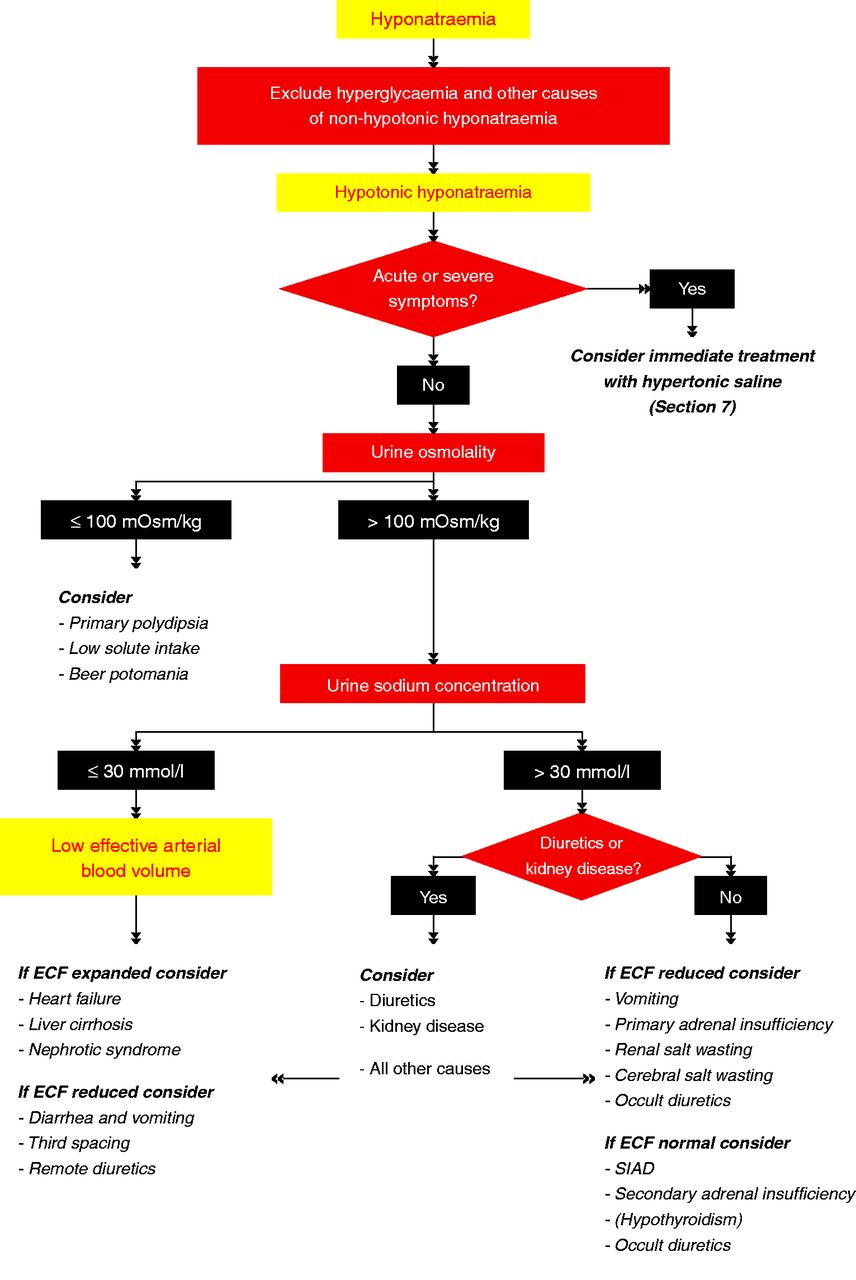
Pour caractériser l’hyponatrémie, il faut obtenir l’osmolalité et le sodium urinaire et se servir de l’algorithme suivant:
Algorithm for the diagnosis of hyponatremia
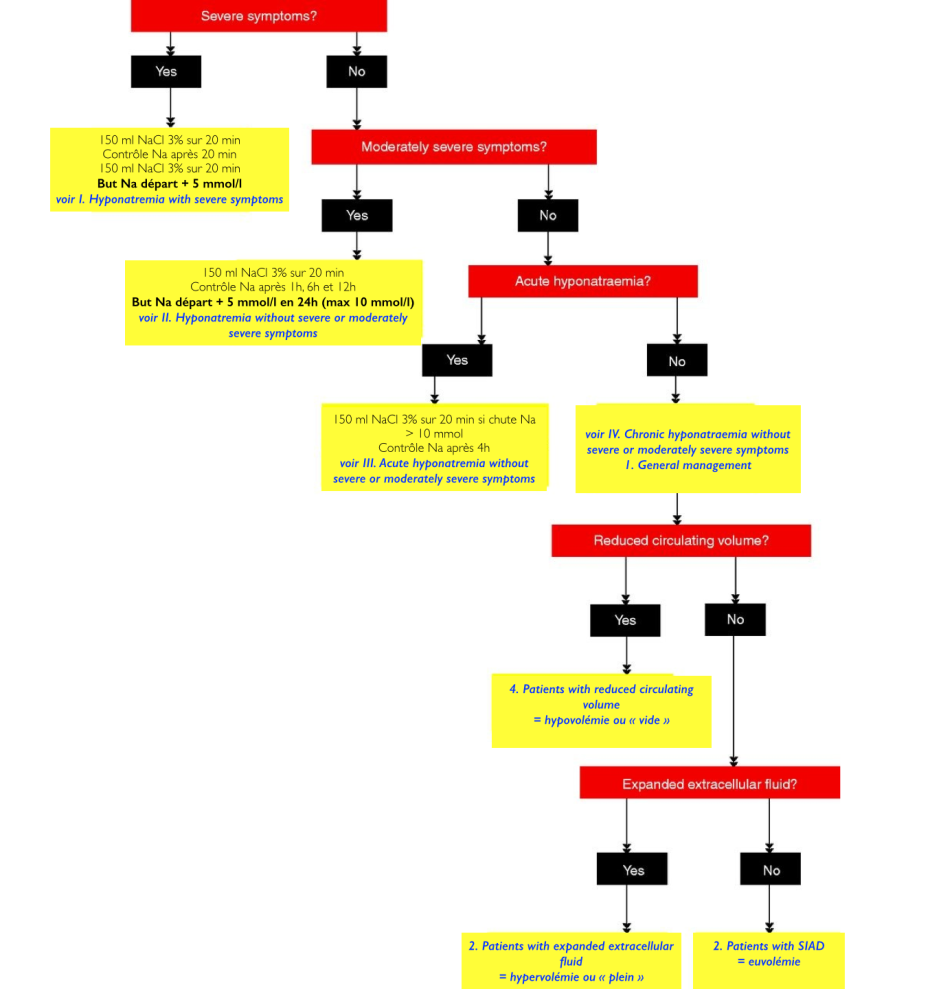
Pour la prise en charge, on a besoin de connaître les symptômes de
son patient, ainsi que la rapidité d’installation de l’hyponatrémie:
Algorithm for the management of hypotonic hyponatraemia
Voici le résumé des recommandations (en anglais)I. Hyponatraemia with severe symptoms
- First-hour management, regardless of whether hyponatraemia is acute or chronic
- We recommend prompt i.v. infusion of 150 ml 3% hypertonic over 20 min (1D)
- We suggest checking the serum sodium concentration after 20 min,
while repeating an infusion of 150 ml 3% hypertonic saline for the next
20 min (2D) - We sugget repeating therapeutic recommendations a. and b. twice or
until a target of 5 mmol/l increase in serum sodium concentration is
achieved (2D) - Manage patient with severely
symptomatic hyponatraemia in an environment where close biochemical and
clinical monitoring can be provided (not graded)
- Follow-up management in
case of improvement of symptoms after a 5 mmil/l increase in serum
sodium concentration in the first hour, regardless of whether
hyponatraemia is acute or chronic
- We recommend stopping the infusion of hypertonic saline (1D)
- We recommend keeping the i.v. line open by infusing the smallest
feasible volume of 0.9% saline until cause-specific treatment is started
(1D) - We recommend starting a diagnostic-specific treatment if available, aiming at least to stabilise sodium concentration (1D)
- We recommend limiting the increase in serum sodium concentration to a
total of 10 mmol/l during the first 24h and an additional 8 mmol/l
during every 24h thereafter until the serum sodium concentration reaches
130 mmol/l (1D) - We suggest checking the serum sodium concentration after 6 and 12h
and daily afterwards until the serum sodium concentration has stabilized
under stable treatment (2D)
- Follow-up management in case of no
improvement of symptoms after a 5 mmil/l increase in serum sodium
concentration in the first hour, regardless of whether hyponatraemia is
acute or chronic
- We recommend continuing an i.v. infusion of 3% hypertonic saline or
equivalent for an additional 1 mmol/l per h increase in serum sodium
concentration (1D) - We recommend stopping the infusion of 3% hypertonic saline or
equivalent when the symptoms improve, the serum sodium concentration
reaches 130 mmol/l, whichever occurs first (1D) - We recommend additional diagnostic exploration for other causes of the symptoms than hyponatraemia (1D)
- We suggest checking the serum sodium concentration every 4h as long
as an i.v. infusion of 3% hypertonic saline or equivalent is continued
(2D)
- We recommend continuing an i.v. infusion of 3% hypertonic saline or
- We recommend starting prompt diagnostic assessment (1D)
- Stop, if possible, medications and other factors that can contribute to or provoke hyponatraemia (not graded)
- We recommend cause-specific treatment (1D)
- We suggest immediate treatment with a single i.v. infusion of 150 ml 3% hypertonic saline or equivalent over 20 min (2D)
- We suggest aiming for a 5 mmol/l per 24-h increase in serum sodium concentration (2D)
- We suggest limiting the increase in serum sodium concentration to 10
mmol/l in the first 24h and 8 mmol/l during every 24h thereafter, until
a serum sodium concentration of 130 mmol/l is reached (2D) - We suggest checking the serum sodium concentration after 1, 6 and 12h (2D)
- We suggest additional diagnostic
exploration for other causes of the symptoms if the symptoms do not
improve with an increase in sodium serum concentration (2D)
- Make sure that the serum sodium
concentration has been measured using the same technique used for the
previous measurement and that no administrative errors in sample
handling have occurred (not graded) - If possible, stop fluids, medications and other factors that can contribute to or provoke hyponatraemia (not graded)
- We recommend starting prompt diagnostic assessment (1D)
- We recommend cause-specific treatment (2D)
- If the acute decrease in serum sodium concentration exceeds 10
mmol/l, we suggest a single i.v. infusion of 150 ml 3% hypertonic saline
or equivalent over 20 min (2D) - We suggest checking the serum sodium concentration after 4h, using the same technique used for the previous measurement (2D)
- General management
- Stop non-essential fluids, medications and other factors that can contribute to or provoke hyponatraemia (not graded)
- We recommend cause-specific treatment (1D)
- In mild hyponatraemia, we suggest against treatment with the sole aim of increasing the serum sodium concentration (2C)
- In moderate or profound hyponatraemia, we recommend avoiding an
increase in serum sodium concentration of > 10 mmol/l during the
first 24h and > 8 mmol/l during every 24h thereafter (1D) - In moderat or profound hyponatraemia, we suggest checking the serum
sodium concentration every 6h until the serum sodium concentration has
stabilized under stable treatment (2D) - In case of unresolved hyponatraemia, reconsider the diagnostic algorithm and ask for expert advice (not graded)
- Patients with expanded extracellular fluid
- We recommend against a treatment with the sole aim of increasing the
serum sodium concentration in mild or moderate hyponatraemia (1C) - We suggest fluid restriction to prevent further fluid overload (2D)
- We recommend against demeclocycline (1D)
- We recommend against a treatment with the sole aim of increasing the
- Patients with SIAD
- In moderate or profound hyponatraemia, we suggest restricting fluid intake at first-line treatment (2D)
- In moderate or profound hyponatraemia, we suggest the following can
be considered equal second-line treatment: increasing solute intake with
0.25-0.5 g/kg per day of urea or a combination of low-dose loop
diuretics and an oral sodium chloride (2D) - In moderate or profound hyponatraemia, we recommend against lithium or demeclocycline (1D)
- In moderate hyponatraemia, we do not recommend vasopressin receptor antagonists (1C)
- In profound hyponatraemia, we recommend against vasopressin receptor antagonists (1C)
- Patients with reduced circulating volume
- We recommend restoring extracellular volume with i.v. infusion of
0.9% saline or a balanced crystalloid solution at 0.5-1 ml/kg per h (1B) - Manage patients with haemodynamic instability in an environment
where close biochemical and clinical monitoring can be provided (not
graded) - In case of haemodynamic instability, the need for rapid fluid
resuscitation overrides the risk of an overly rapid increase in serum
sodium concentration (not graded)
- We recommend restoring extracellular volume with i.v. infusion of
Source
1.Clinical practice guideline on diagnosis and treatment of hyponatraemia Eur J Endocrinol 2014
Aucun commentaire:
Enregistrer un commentaire